Osteoarthritis
Osteoarthritis is a condition that affects the joints, causing pain and stiffness. It is the most common form of arthritis and occurs in people all over the world. It is also known as degenerative arthritis.
A joint is the point where two or more bones come together. Joints allow bones to move freely up to certain limits.
When a joint is affected by
osteoarthritis, its surface is damaged and it does not move as it should. The following happens:
- The cartilage becomes rough and thin.
- The bone at the edge of the joint begins to grow outwards and forms bone morphs called osteophytes.
- The synovial membrane may swell and produce fluid, causing swelling in the joint.
- The joint capsule and ligaments gradually harden and contract.
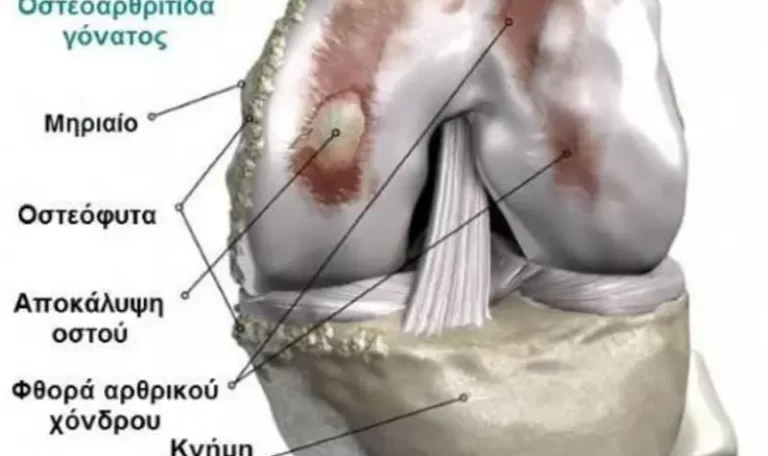
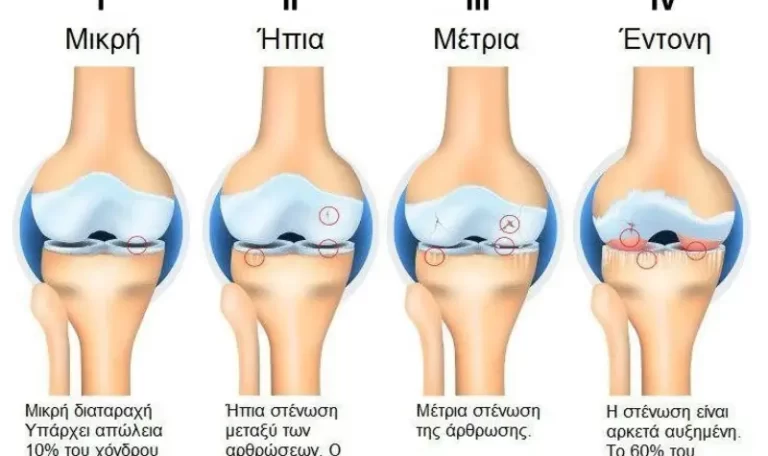
In cases of severe osteoarthritis, the cartilage becomes so thin that the bones begin to rub together and wear out. Cartilage loss, bone wear and bone spurs can change the shape of the joint, causing the bones to shift from their normal position.
The symptoms are:
- Pain
- Stiffness
- Creaking when moving the joint
- Chewy or hard swellings
The main symptoms of osteoarthritis are:
- Pain (especially when moving the joint or at the end of the day)
- Stiffness (especially after rest, however it passes after a few minutes of movement)
- Creaking when moving the joint
- Hard swelling (caused by osteophytes)
- Yeast swelling (caused by fluid accumulation in the joint)
Osteoarthritis in the knee
Knees are affected by osteoarthritis more often than any other joint. The reason is that they are subjected to excessive stress, bending and twisting. Osteoarthritis affects the main surfaces of the knee joint, as well as the cartilage under the kneecap.
Usually, it affects both knees, and patients experience pain in the front and side of the knees.
Severe osteoarthritis can cause ravogony (a gap between the knees). The joints in the knee become unstable and give way as soon as they receive weight. This is due to muscle weakness or damage to the ligaments.
Who is at risk?
Osteoarthritis in the knee usually affects:
- Women – women are twice as likely to get osteoarthritis in the knee as men
- People over 55
- Overweight people
- People with nodular osteoarthritis (especially women)
- People who have suffered a sports injury in the past (torn meniscus or ligament)
- People who have had surgery to repair a meniscus tear (meniscectomy)
Anyone can get osteoarthritis, but the risk increases for:
- People over 45
- Overweight people
- Women
- People whose parents were affected
- People who have had a joint injury in the past
- People who have had joint damage from another disease (e.g. gout or rheumatoid arthritis)

Many factors can increase the risk of osteoarthritis. It occurs most often in:
- People over 45
- This may be because the muscles become weaker or the joints gradually wear out.
- Women
- Osteoarthritis, especially in the hands or knees, occurs more often and in a more severe form in women.
- Overweight people
- Weight increases the likelihood of osteoarthritis, especially in the knees, and makes the condition worse.
- People whose parents were affected by osteoarthritis
- Nodular osteoarthritis, which affects the hands of middle-aged women, is hereditary. Some rare forms of osteoarthritis, which start at an early age, are linked to genes that affect collagen, which is a key component of cartilage. Gene factors play a smaller, but equally important, role in osteoarthritis of the hip and knee.
- People who have had a joint injury in the past
- Severe injury or surgery to a joint may cause osteoarthritis in that joint.
- Difficult, repetitive activity or exhausting work increases the risk of getting sick.
- People with congenital or acquired deformity of a joint
- This may lead to more severe forms of osteoarthritis, which may occur at younger ages than usual.
- People suffering from an arthropathy
- Osteoarthritis can occur from damage due to another arthritis, such as rheumatoid arthritis or gout.
Osteoarthritis in the hands
Osteoarthritis can affect any joint, especially if it has been injured in the past. It occurs most often in the following joints:
- Knees
- Ishia
- Hands
- Neck and waist
- Big toes
- Shoulder
Osteoarthritis in the hands usually comes from nodular osteoarthritis. It mainly affects the base of the thumb and the joints at the fingertips.
However, it can also affect other joints of the fingers. The joints become swollen, irritated and sensitive, especially when the joint first appears
disease. Over the years, solid lumps develop on the back of the finger joints. These lumps are called Heberden’s nodules. Often, the pain and tenderness subside once the nodules are fully developed. The fingers usually function normally, despite the bumps or slight bending. The joint at the base of the thumb may continue to cause problems.
Who is at risk?
It usually offends:
- Women
- People between 40 and 60 years old (around the time of menopause)
- People whose parents (especially the mother) were affected by the disease – nodular osteoarthritis is more hereditary than other forms of osteoarthritis
Patients who were affected by nodular osteoarthritis when they were middle-aged are more likely to develop osteoarthritis in the knee and possibly other joints.
Treatment varies depending on how severe the pain is. A combination of over-the-counter analgesics and self-help methods is usually enough.
However, if the pain is very severe, the doctor may suggest some of the following treatments:
- Capsaicin cream
- Strong analgesics (e.g. tramadol) for more severe pain
- Cortisone injections in the painful joints
- Transcutaneous electrical nerve stimulation (TENS)
- Surgical treatment, including joint replacement
There is still no cure for osteoarthritis. But there are treatments that soothe the symptoms and reduce the likelihood of worsening
arthritis.
Pills and creams
Analgesics relieve pain and stiffness, but they do not affect the arthritis and do not repair the joint damage.
- It is only recommended to administer them when the pain is severe or the patient is going to exercise.
- Usually paracetamol (Depon or Panadol) is the best and best tolerated analgesic. However, it must be given at the correct dose, as many patients take a reduced dose. It is recommended that 1 gram (usually 2 pills) be given 3 or 4 times a day.
- Combination analgesics (e.g. paracetamol and codeine or paracetamol and dihydrocodeine) contain paracetamol and some form of codeine, and are indicated for very severe pain. Because they are stronger analgesics, they may cause side effects such as dizziness and constipation.
- Non-steroidal anti-inflammatory creams and gels are a good alternative for those who have problems with NSAID pills. They help quite a bit with osteoarthritis in the knee or arm, but not in deep joints such as the hip.
- In case of very severe pain, and if other drugs are not effective, stronger analgesics (e.g. opioids/anti-inflammatories) may be given.
Other treatments
Heat or cold sometimes provide relief from pain and stiffness in the joints.
- Heat lamps are quite popular, but hot water bottles or heated pads (sold in pharmacies) are just as effective.
- Ice packs also offer relief from pain.
- Hot or cold compresses should not come into direct contact with the skin.
Intra-articular cortisone injections are sometimes recommended for particularly painful joints.
The injections work in one to two days and relieve pain for several weeks or months, especially in the knee or thumb.


